Published on 5 November 2024
AI in Medical Education
Professor Joseph Sung
Distinguished University Professor
Senior Vice-President (Health & Life Sciences)
Dean, Lee Kong Chian School of Medicine
The rapid advancement of Artificial Intelligence (AI) is reshaping healthcare, creating new opportunities and challenges. Traditionally, medical education has focused heavily on basic sciences and clinical practice. However, as AI technology continues to evolve, it’s clear that this approach must adapt. The healthcare professionals of tomorrow will need skills that prepare them to work effectively alongside AI, using it to enhance patient outcomes and drive innovation in care delivery.
AI is becoming integral in diagnostics, treatment planning, and patient care. Machine learning algorithms can now analyse medical images, predict disease patterns, and help personalise treatment plans based on patient data. For instance, AI in radiology and pathology is fast developing, assisting clinicians in interpreting complex images and identifying diseases at early stages. Yet, AI is not, and should not be, a replacement for doctors—it’s an assistive tool that can handle repetitive and mundane tasks, freeing physicians to focus on critical decision-making and patient relationships.
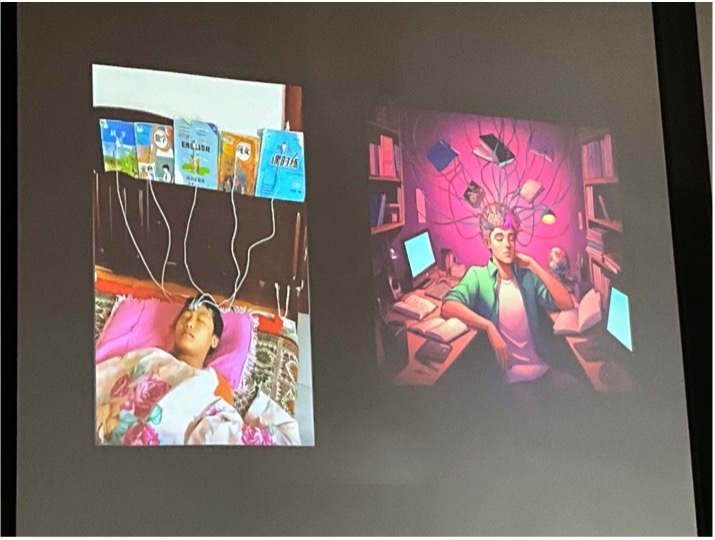
Today’s medical curricula emphasise memorisation, clinical skills, and diagnosis, with limited attention to technology-driven competencies. However, memorising facts may be less relevant in an era where AI can rapidly access and analyse vast amounts of medical data. Meanwhile, critical skills like digital health literacy, data interpretation, and the ethical implications of AI in healthcare remain under-represented. This gap between traditional training and emerging healthcare needs underscores the urgency of curriculum reform.
To prepare students for the future, medical education must incorporate AI, data science, and technology in meaningful ways. Courses on AI fundamentals, machine learning, and data interpretation can equip students to use AI tools effectively and responsibly. Additionally, training on AI ethics and bias is crucial to ensure that future clinicians understand the ethical challenges posed by AI and work toward equitable, patient-centred care. Emphasis should also be placed on developing skills that AI cannot replace, such as empathy, complex problem-solving, and patient communication. By honing these uniquely human capabilities, future physicians will be better equipped to use AI while providing compassionate care.
Some medical schools are already piloting AI-enhanced learning tools, such as virtual simulations and augmented reality, which allow students to gain experience in a controlled environment. AI-driven tutoring systems can personalise learning experiences by adapting to each student’s strengths and areas for improvement. Additionally, interdisciplinary collaborations with fields like computer science and bioinformatics provide a broader context for understanding AI applications in medicine. Stanford offers courses on AI and machine learning applications in medicine, covering topics like predictive analytics, data-driven diagnostics, and genomics. Students can also take interdisciplinary courses with the Stanford AI Lab, focusing on real-world applications and ethical considerations of AI in healthcare. University of Toronto has introduced courses and workshops on AI, machine learning, and data science tailored specifically for medical students. Their programmes include hands-on projects where students work on analysing healthcare data and exploring AI-driven diagnostic tools. They also emphasise ethical considerations and responsible AI use in patient care. Harvard offers a programme called "AI in Medicine," a collaboration between the medical school and the Harvard-MIT Center for Regulatory Science. This initiative includes modules on AI applications in medical imaging, clinical decision support systems, and drug development. Harvard also focuses on teaching students about AI limitations and the ethical challenges surrounding AI in clinical practice. These programmes represent an evolving approach to medical education, where future physicians are trained not only in clinical skills but also in digital health literacy, data science, and the ethical dimensions of AI. Through such initiatives, these schools are preparing students to embrace AI as a complementary tool, enhancing patient care while remaining aware of AI’s potential limitations and biases. To stay relevant, LKCMedicine too is working with the College of Computing and Data Science of NTU to offer such courses in our MBBS curriculum.
Besides teaching how to use AI in future clinical practice, AI tools are also transforming how medical education is delivered, offering personalised learning experiences, enhanced simulations, and data-driven insights. There are many AI-powered adaptive learning platforms available. Smart Sparrow is an adaptive learning platform that uses AI to tailor learning experiences for students. It provides personalised feedback and customises content based on individual progress, allowing students to focus on areas where they need improvement. Body Interact and Sim-X use VR and AI to create immersive, scenario-based training for medical students. It covers various clinical scenarios, helping students practise diagnosis, treatment planning, and patient management in realistic settings. We are exploring the use of such devices for teaching at LKCMedicine.
I’m confident that integrating AI into medical education will future-proof our profession, equipping new doctors with the skills they need to thrive in an AI-augmented healthcare system. By embracing this change, we can shape a new generation of healthcare professionals who are skilled, adaptable, and ready to leverage technology to enhance patient care and drive the field forward.

