NTU Singapore develops peptide that makes drug-resistant bacteria sensitive to antibiotics again
Scientists at NTU Singapore have developed a synthetic peptide that can make multidrug-resistant bacteria sensitive to antibiotics again when used together with traditional antibiotics, offering hope for the prospect of a combination treatment strategy to tackle certain antibiotic-tolerant infections.
On its own, the synthetic antimicrobial peptide can also kill bacteria that have grown resistant to antibiotics.
Every year, an estimated 700,000 people globally die of antibiotic-resistant diseases, according to the World Health Organisation. In the absence of new therapeutics, infections caused by resistant superbugs could kill an additional 10 million people each year worldwide by 2050, surpassing cancer. Antibiotic resistance arises in bacteria when they can recognise and prevent drugs that would otherwise kill them, from passing through their cell wall.
This threat is accelerated by the developing COVID-19 pandemic, with patients admitted to hospitals often receiving antibiotics to keep secondary bacterial infections in check, amplifying the opportunity for resistant pathogens to emerge and spread.
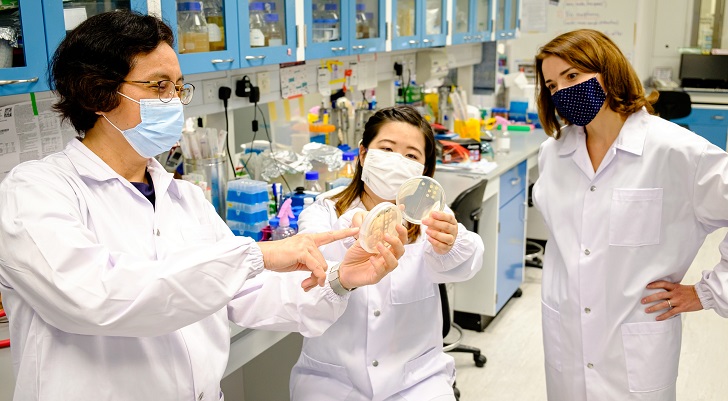
The NTU Singapore team, led by Associate Professor Kimberly Kline and Professor Mary Chan, developed an antimicrobial peptide known as CSM5-K5 comprising repeated units of chitosan, a sugar found in crustacean shells that bears structural resemblance to the bacterial cell wall, and repeated units of the amino acid lysine.
The scientists believe that chitosan’s structural similarity to the bacterial cell wall helps the peptide interact with and embed itself in it, causing defects in the wall and membrane that eventually kill the bacteria.
The NTU Singapore team, led by Associate Professor Kimberly Kline and Professor Mary Chan, developed an antimicrobial peptide known as CSM5-K5 comprising repeated units of chitosan, a sugar found in crustacean shells that bears structural resemblance to the bacterial cell wall, and repeated units of the amino acid lysine.
The scientists believe that chitosan’s structural similarity to the bacterial cell wall helps the peptide interact with and embed itself in it, causing defects in the wall and membrane that eventually kill the bacteria.





5872e661-3cf5-41b6-abee-8d297a83209c.tmb-listing.jpg?Culture=en&sfvrsn=61d1c8d7_1)